In our last installment of this series, I’d like to review some of the ongoing changes in our healthcare system and their potential impact on how healthcare is practiced in US.
First, health insurance exchanges are meant to provide everyone an opportunity to have health insurance. On the surface, this might suggest increased costs to the government since many people will receive government subsidies to buy health insurance. How, then, does this help the government save money and stay solvent? Well, many of these people are currently getting care in very expensive settings such as emergency departments or hospitals, and cost the system lots of money.
This results in rise of the healthcare costs and everyone ends up paying more, including the government. By insuring everyone, the goal is that people will get preventive care and have access to the system before they need to go into the emergency departments or hospitals. This will result in lowering the overall cost of care. The Congressional Budget Office (CBO) projects that this will result in significant reductions in overall healthcare costs over the next few decades.
Second, payment reform will mean that providers will need to shift from getting paid per episode of care to payment based on the outcome of their actions. This is quite a change from how medicine has been practiced and paid for historically. Providers are used to seeing their patients when those patients feel that they need medical care. After each episode of care, be it in a clinic or in a hospital, patients and their families are responsible for following the medical instructions.
Now, with the new payment models, providers need to worry whether their patients will fill their prescriptions or take them. They’ll need to identify their high-risk patients, anticipate their complications, and intervene before they reach a critical stage where they may need expensive care in a hospital.
How are providers dealing with this? Many are taking very measured steps toward these new care delivery models. Change is not easy but you have to start somewhere. Since these programs were pioneered and expanded, they have shown mixed results and many providers have struggled to show results.
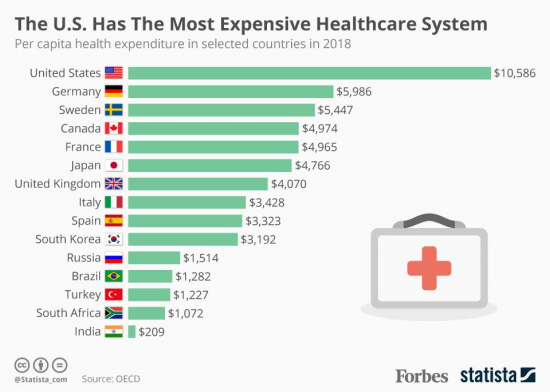
What is clear is that the healthcare system in the US costs more and shows worse outcomes than many of its peer countries. Objectives measures such as infant mortality and life expectancy in US lag other industrialized nations while cost of care per capita is much higher here. That is because of the fact that there are significant wealth and income disparities in US, universal health insurance is not available, and social programs such as nutrition for the poor and children are not as robust in the US than in western Europe, Australia, or Japan. In other words, the disparities in health outcomes and cost of care are not just related to the healthcare system in the US but also to our entire economic system.
The US health system has much to be proud of and many of the innovations being tried here will catch fire in other places. As a matter of fact, if history is any indication, many of those countries will do a much better job of making some of those innovations a reality. What I hope will happen is that someday we can also learn from other countries in how they manage to keep their people healthier at a much lower cost than us. Most of these countries are capitalistic countries like us and can’t be called socialist countries, which is a common response when you suggest making some changes to improve our system (and do crazy things like learning from the success of others!)
Many reforms will need to be made to bring the overall outcome of our healthcare system on par with other industrialized nations but a few fundamental adjustments such as universal health insurance, support for children’s nutrition and health education, and increasing government support for education, R&D, and infrastructure (the type of programs that lead to long-term increase in jobs and higher wages for middle and working class people) can go a long way to address many of these issues.