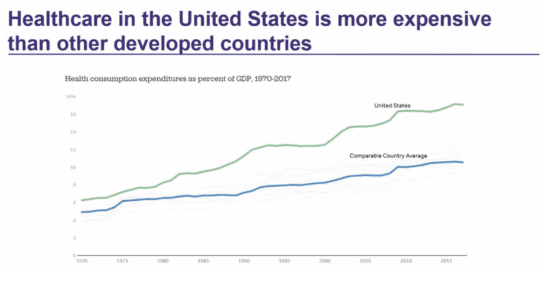
THE US HEALTHCARE ECONOMY is valued at almost $4 trillion. If it was a country, it would have the fifth largest economy in the world, and it equates to nearly half of what the entire world spends on healthcare. We can argue about whether that’s a good thing or not and what percentage of it is actually necessary, but we can all agree that it’s an inefficient system. It’s convoluted and the overall setup creates redundancies and needs lots of approvals and what we used to call paperwork. In fact, it’s estimated that about 25% of this $4 trillion is due to administration, which means that we spend $1 trillion a year on paperwork. It’s no wonder that healthcare is now the number one employer, passing retail as of 2017 with 17 million jobs.
Administrative money needs to be spent to support activities outside of direct patient care. Given that most economies in the world are smaller than $1 trillion, you could say that the administrative part of the US healthcare system is also one of the largest economies in the world. Part of that is because we have more than 1,000 insurance companies, each with its own policies and forms, requiring a major revenue cycle function in each hospital system and even in small doctors’ medical clinics. A typical medical clinic or health system has to deal with so many different payers that many of its employees are occupied with filling out forms and making calls to ensure that they’re meeting each payer’s requirements, because that’s what pays the bills and keeps the lights on. When we think of care delivery institutions, this isn’t what typically comes to mind. Unfortunately, it’s a reality because of the disjointed payment system in our country and the lack of regulation to solve the problem.
Another contributing factor is the lack of an efficient source of longitudinal patient medical records which would simplify data sharing and access of information for providers, commonly referred to as a health information exchange (HIE). A single national healthcare database could be achieved through either a commercial or government program that would ensure that all healthcare providers had access to the same data for patients instead of having to waste resources searching for and retrieving data from other institutions.
All of this means that both payers and providers have to expend tremendous resources on administrative tasks. The good news is that we can expect to see future workflow improvements through robotic process automation (RPA), artificial intelligence (AI) and other promising technologies. These technologies are a natural fit to improve efficiency through automating repetitive tasks with minor or moderate complexity. In the next few posts, we will discuss how AI can start to improve the consequences of a fragmented system.