Most of the administrative functions in healthcare are done electronically nowadays, making AI the perfect tool to “figure out” what to do and to perform activities like completing forms, sending information and scheduling follow-ups. This would bring three economic improvements to the process: first, it would mean fewer healthcare resources, including the time of doctors and nurses, spent on administration; second, it would enable more timely completion of these steps and reduce the time to achieve revenues; and third, for the same budget, it would enable the allocation of more money for actual patient care.
As Rock Health put it in their report about AI in healthcare: “Media has largely centered on the ability of AI/ML to transform how clinical care is delivered through better diagnostics and treatments. But AI/ML is even more quickly transforming the business of healthcare through the automation and enhancement of non-clinical, operational functions—such as claims adjudication, patient engagement, scheduling optimization, risk analytics and documentation.”
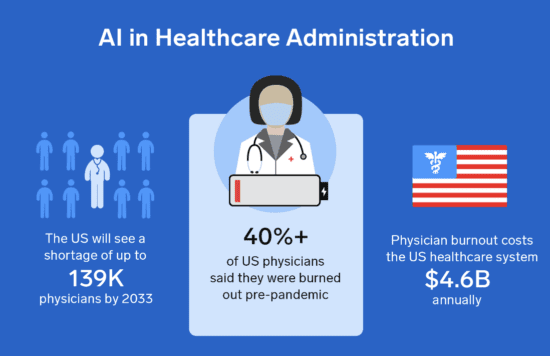
These AI systems could also help us to reduce burnout amongst physicians that’s brought on by the ever-increasing need for doctors to carry out administrative tasks like coding, claims, pharmacy refills and pre-authorization. Carrying out these manual, repetitive tasks for billing and insurance is frustrating for physicians and costly for healthcare providers. That’s why the ability of AI to reduce these tedious and time-consuming workflows in the backend could be one of its biggest impacts in the healthcare industry. It’s estimated that AI could lead to time savings of 17% for doctors and over 50% for nurses.
The administrative staff of medical institutions deal with a range of revenue generating activities in support of medical care, like verifying patients’ insurance eligibility, identifying the right medical codes based on the services provided, submitting claims to insurers and following up with patients about outstanding bills. With advances in AI technologies such as computer vision and machine learning-enabled bots, many of these activities can be intelligently automated. Robotic process automation (RPA), an umbrella term for automating repetitive back-office tasks like onboarding and document digitization, has especially benefited from advances in computer vision and natural language processing. This is very relevant to the major issue of excessive administrative costs. Given that the technology finally seems ready for its moment, more hospitals are weighing the benefits of using AI for coding and billing automation.
Managing billing, revenue collection, insurance filings and other related activities is at the frontier of AI’s entry into healthcare. That’s because it’s a low-risk area with an immediate financial impact for the health system. It doesn’t carry the liability risks of clinical AI applications, where small errors could have large consequences on patient outcomes. Furthermore, medical providers don’t need to worry about securing reimbursement, and the business case is much more compelling in the short-to-medium term than clinical AI applications.