For anyone that has dealt with the US healthcare system in any way imaginable, there’s mounting frustration. For those of us who have sought care for various issues, we know that barriers and confusion await you at almost every turn: getting to see a PCP or the right specialist entails long wait times; when you do see someone they may not have everything they need to properly care for you as parts of your records may be sitting in multiple other clinics or centers; the doctors are not necessarily focusing on you so much as stirring at their computer screen and typing; submitting forms to your insurance company to approve any needed diagnostics or procedures; having to fight the denials of needed care and waiting and worrying about it all; long wait times to get on the schedule for those tests and procedures; not really understanding what is going on given that the doctors have limited time to keep explaining things in a way that we can follow and understand, and much more. If I’m painting too vivid of a picture, I apologize, for the understatement!
Since the passage of the Affordable Care Act in 2009, mandating of the Electronic Health Records (EHR,) and the push for Value-based Care at the same time, there has been optimism that policy plus technology plus a culture of innovation in US will finally start addressing some of these issues. Well, here we are 16 years later and frustration with our system is at an all time high. And, the output of our system has not improved much. We continue to be laggards amongst the advanced nations in our health outcomes and we spend more per capita than any other nation. In my first two articles of 2026, one in this blog and another in Fast Company, I discuss these dynamics and how the legislative and regulatory changes in 2025 can intensify existing problems. As people lose coverage due to the Medicaid cuts and expiration of enhanced ACA subsidies, more people will show up to ERs for routine care, driving up costs and clogging up precious resources. In this environment, healthcare providers will face budgetary issues as they will need to provide care that is not reimbursed (higher number of the uninsured) and lower reimbursement for the care they do provide. This will limit their ability to engage in care model transformation and investing in technologies that will address some of the mentioned issues.
It’s against this backdrop that I present my hypothesis: given the worsening policy and fiscal environment for healthcare providers, on top of the fact that even in the best of times they are slow in adopting innovation that can improve the experience and quality of the healthcare, is it time to start innovating outside of the existing system? This, of course, has been tried before with many direct to consumer health offerings attempting to create new pathways for people to receive certain types of care. A good example of this has been the retail clinics that have been created within pharmacies like CVS and Walgreen or retailers like Walmart. The entire concept of these clinics was easier access, lower costs, and more convenience. You can say that they were trying to divert some of the traffic from the traditional providers to a new clinic concept. So, what is the result to date of this very reasonable concept? Well, not good! Most of these clinics have actually been shut down or scaled back. It seems that it’s not necessarily easy to see enough episodes of care through to completion. Many frontline quick diagnostics or short visits turn into more complicated encounters that these clinics are not set up for. As many as 40% of the patients ended up needing to be referred to actual medical centers for more testing and treatment. This has led in some instances to more fragmentation of care and duplication of testing and hence increased costs.
While that doesn’t seem very encouraging, and we have also seen this with many online D2C offerings, we may be at a moment in time that technology may help us break this case open. The key driver of most of the issues with our healthcare system is a shortage of resources. An aging population, not having trained enough clinical people over the last couple of decades, and increased consumerization in healthcare have landed us in this place. It is not conceivable that we can get out of this jam without technology coming to the rescue. This also has been a trouble spot for healthcare: while many sectors of the economy like travel, banking, and hospitality were significantly transformed by the internet and software, the same did not happen in healthcare. As a matter of fact, the most important technology that was adopted in healthcare over the last 20 years, EHRs, are viewed as technology that did not really improve experience or quality for providers or patients.
Why has healthcare been so immune to the benefits of technology? The main reason, in my opinion, is that automation of processes in healthcare is more difficult than other sectors. This is mostly because you’re dealing with multimodal data: images, reports, labs, clinical notes, genetics, etc, and historically we have not had technology that can read all of this different types of data in combination, identify meaning and patterns, and take action based on that. This is true across operational, administrative, and clinical areas of healthcare. Each one of these requires processing complex multimodal data, much of it unstructured. We may be at the dawn of an age where transformer-based AI models can do an acceptable job with this and finally introduce some automation. We’re seeing that with some of the applications that are gaining adoption such as ambient documentation, revenue cycle management solutions, and clinical decision support. This is relief inside of our system and there is, at least, anecdotal report of improved experience and possible financial ROI.
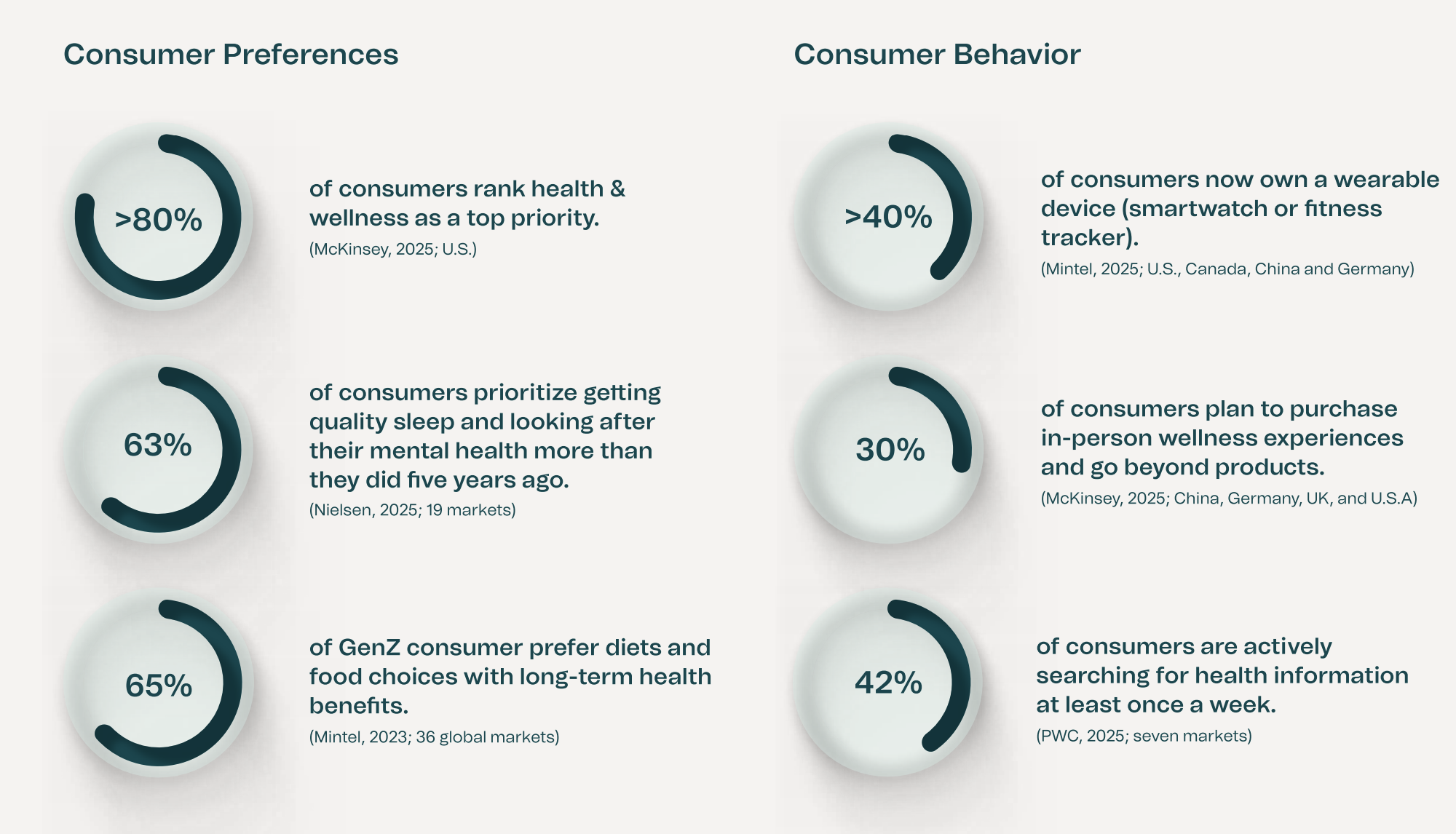
While the industry learns about these technologies and goes through their protracted selection and implementation processes, there may an opportunity to start improving the system from the outside. Consumer health AI products that can use people’s data to identify risks and help them with managing those risks may not be far off. As people gain more access to their own clinical data through portals and smart phone apps, coupled with ongoing data collection through wearables, apps, home testing, and more, this vision can become a reality. Much of the shortage in our system can be relieved with appropriate triage of developing issues to lower cost settings and personalized guidance that prevents unnecessary visits. Combine that with true prevention that results from ongoing monitoring of the health data and providing lifestyle nudges that can alter health trajectories and now you’re talking about improvements in long-term outcomes and cost reduction. While these goals have been aspirational for decades, emerging technologies may be bringing them closer to reality. Creating something like this is not easy and will require robust infrastructure While this may not be right around the corner, given the increasing interest in health topics among all generations, more access to clinical data, rise in wearables use, and increased willingness to pay out of pocket, it may not be that far off.
Given the enormity of the issues facing our healthcare system, thinking outside the box and leveraging the improving capabilities of AI may be how we achieve a breakthrough.





