If the first decade of digital health has taught us anything, it’s that having an innovative product does not necessarily mean success. There are many problems in healthcare and there are technologies today for many of those issues. So why are those technologies not being used to solve those problems? Well, because bringing digital technologies into healthcare is very difficult. When you introduce a new digital technology into a clinical workflow or a pharma company, it’s almost never invisible. It will mean that a new workflow has to be introduced for the users. There may be great overall benefits for the technology but the users may not like the new workflows and resist adopting it.
Enter Electronic Health Records! Although everyone ultimately ended up using an EHR because it was mandated by the government, the users have never taken to using them. They create extra work and provide very little benefit beyond having the data digitized. Now, that’s a hug benefit and the next generation of solutions are only possible because the data is digital, but for ages it was not possible to drive their adoption because of these issues.
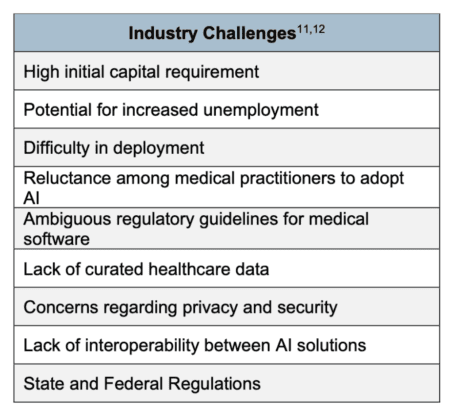
The next generation of digital solutions, including AI-powered ones, will not have a government mandate behind them. As such, whether they will see adoption will depend on several factors, including their workflow implications. Other factors that are critical for the adoption of digital technologies in healthcare include the nature of the problem they’re solving, the importance of that problem, the proposed magnitude of the impact of the new solution, the complexity of their implementation, reimbursement prospects, and more. Once you see this list, you realize why most digital health tools have not had success in gaining adoption or achieving scale. These are a lot of issues to navigate. And, if you check every box, you may still not make the cut because of the limited technology budget at most institutions and how those dollars are usually spent on the most urgent issues, such as EHR upgrades or improving the existing infrastructure.
So, what is the business case for these technologies? How do you ensure that if you’re building something, you’re not wasting your time? I only know of one approach and that is to analyze these issues extensively before taking on years of development. Many technologies that sound promising face significant challenges in one or several of these areas. That means once you build them, the commercialization efforts will not be easy and in most cases, too challenging to be worth it. As you can see from the list, anything other than extensive analysis by interviewing potential users, buyers, maybe payers, and more will not be enough. In many cases, this research may cover other opportunities that would be better solutions to develop.
For the potential buyers of these technologies, the same analysis makes sense. After-all, if the economic benefits are not large enough, it is doubtful that any piece of technology will be prioritized given the limited budgets. If the users won’t take to the new workflows, buying the technology won’t lead to adoption. If the data needed for the solution to work resides in too many disparate systems, it won’t be able to create the desired output in production. Will insurance companies reimburse for using it if one of the key value propositions is better patient outcomes? That can make or break your commercial plans.
Over the next new posts, we will tackle these issues and how to analyze them if you are a builder, buyer, or investor in digital health/health AI technologies.