Chronic disease management is complicated and onerous, both for the care team and for the patients. Most chronic disease management programs haven’t shown significant ROI. It’s a daily process that requires attention, follow-through, follow-ups, and ongoing communication. Most patients don’t have the time or patience for it and most care teams don’t have enough resources to do it well. A lot of chronic disease management comes down to figuring out how the patient is doing with their disease and addressing any issues. This is laborious and time-consuming, but if you dissect it carefully enough, you can see that we’re increasingly using tools that can automate much of it.
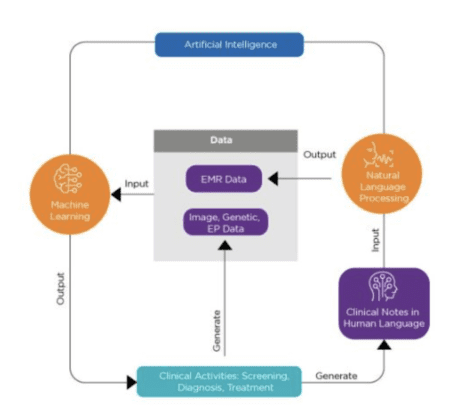
Data collection is getting much more streamlined thanks to sensors, cell phones, wearables, interactive questionnaires and other tools. Basic decision support software is now being used for both patients and providers. These decision support software applications are currently mostly rules-based and limited in what they can do, but they’re good for first-line support and can obviate the need for the care team to get involved with basic tasks. The next generation of decision support software could be powered by AI, trained on large sets of data and similar scenarios with the outcomes identified for it to learn from. This means that it will be much more dynamic in its assessments. It’s not as though this will be available to us tomorrow, but some versions of it are already being rolled out.
One example of this is in diabetes. Due to the explosion of obesity in the US (and the rest of the world), this is now a disease that’s consuming major resources and dollars in our healthcare system. Diabetes management requires monitoring blood glucose on a daily basis and adjusting the patient’s treatment, sometime daily if they’re taking insulin. This perfect for AI: identifying patterns in long-term data and making recommendations on what should be done next to optimize for the defined outcomes. AI solutions can make treatment recommendations based on the analysis of how thousands and millions of patients have responded to different treatments.
Recently, the University of Utah Health, the Regenstrief Institute and Hitachi announced the development of a new artificial intelligence approach that could improve treatment for patients with Type 2 diabetes mellitus. Researchers from all three organizations collaborated to develop and test a new AI approach to analyzing EHR data across Utah and Indiana. As they did so, they uncovered some patterns for Type 2 diabetes patients with similar characteristics. The hope is that those patterns can now be used to help determine optimal drug regimens for specific patients.