While there are great steps being taken in every part of the health innovation economy, one question that always comes to mind is how much of these innovations are actually making it to the frontlines of care? If you read the literature in this field, it’s full of stories of success about the use of technology to help with the patient experience or clinician burnout or clinical outcomes or higher collection rates, and more. Yet, when you get out there and speak with people who work in various healthcare institutions, you get the sense that many organizations are still very early in their journey with these technologies, including AI. That can be surprising given everything all of us read on a regular basis about the potential of technologies like AI, not just in healthcare but across the economy. But it’s not just the potential of AI that we read about, it’s also how many organizations have had success in moving the needle in business and clinical outcomes using these technologies. So, what’s the verdict?
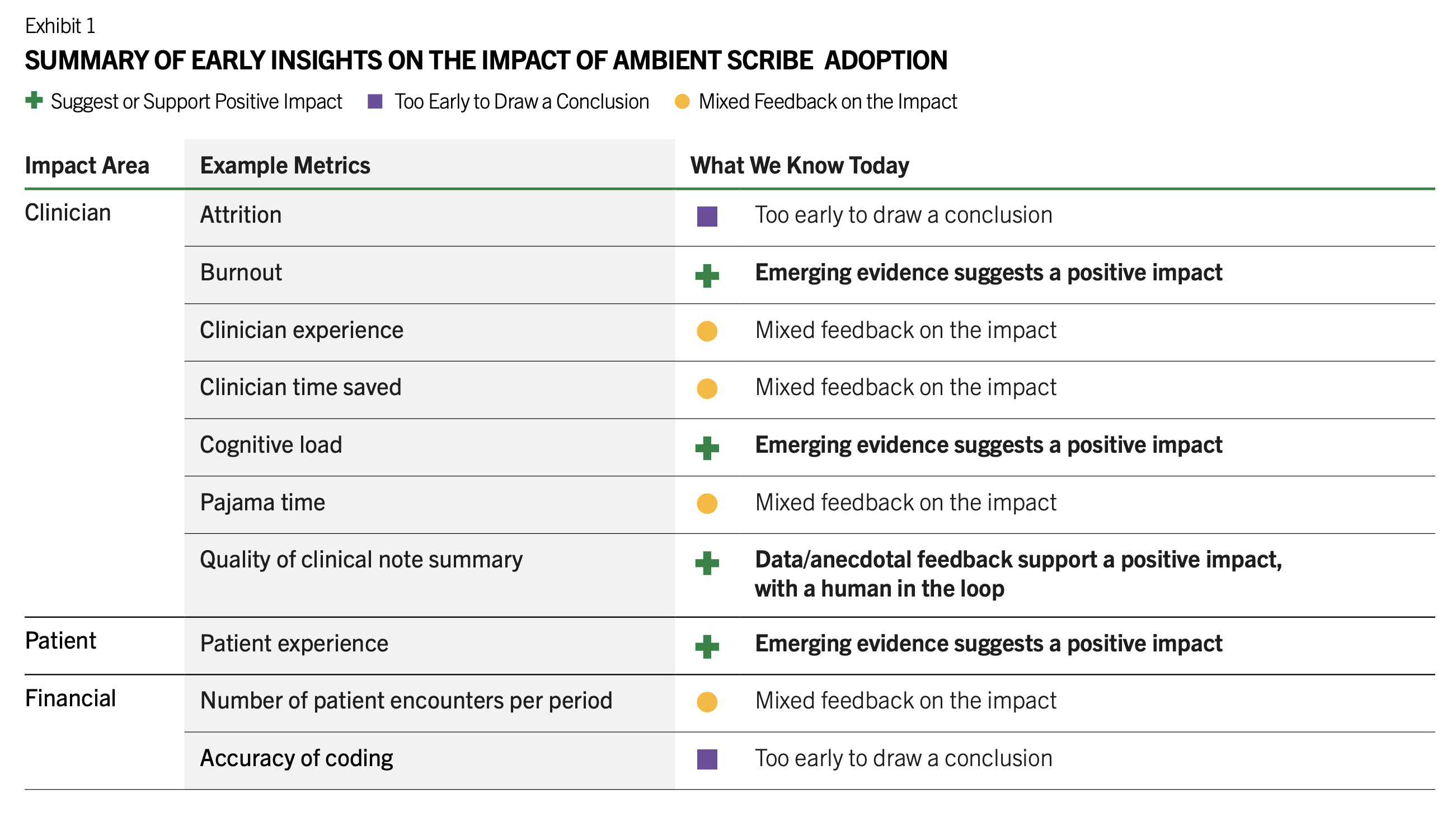
A careful examination of the recent surveys and articles, coupled with personal discussions with a large number of operators out there gives me the sense that most organizations are still at the early stages with technologies like AI. While there are many pilots underway, most have not yet scaled up these technologies due to a variety of reasons. There are certain use cases, mainly ambient documentation and co-pilot inside the EHR, that are gaining rapid adoption. It’s hard to think that any doctors would want to go back to writing notes once the notes are automatically generated for them by AI. But, for the next few years that this use case will go through its rapid adoption phase, many physicians will resist changing their habits. Many have created templates for their notes and don’t want to move off of those. Also, the cost will be a factor for many provider institutions. Since unlike many previous technologies, AI can actually complete an activity end-to-end, usage- or output-based pricing is becoming more common with AI vendors, as opposed to pricing per user or seat. While this will be advantageous for the technology firms, it’s not great for their customers who may end up with hefty bills if the usage skyrockets in their institutions.
One of the factors that is causing confusion and delays in decision making by the healthcare executives is the vast number of use cases and technologies out there, all of which claim to improve business or patient outcomes, address staff burnout, and improve experience. Most do not have solid evidence to support their claims but it does not keep them from showing up with spreadsheets full of impressive numbers that show increased revenues and lower costs for providers. Are these numbers based on large number of customers or users? No, because most do not have large numbers of users yet. Even ambient documentation, which we can say is the first AI use case in healthcare to demonstrate wide scale adoption, has not yet definitely shown financial ROI but is showing lower documentation times per doctor that is meaningful given the shortage of providers and the high burnout rate. All of this means that marching into an executive’s office with lofty claims about your brand new shiny health AI solution may not get the warm reception that you’ve hoped for! As such, the first step in all of this will need to be the education of the executives that are in charge of buying these technologies for their centers. The more you can connect the value of your technology to their critical business issues, the better chance you have that they will consider giving you a try.
Moving down from the executive ranks to the IT departments, the next level of issues to deal with are a range of technical challenges. First and most important are the data issues. As I write in my book, AI Doctor, the state of data in healthcare is a major barrier to the brisk adoption of AI. Given that almost all of us get our medical care from different providers and thus, they each have a piece of our health data. Even within a large institution like a health system that has multiple hospitals, clinics, imaging centers, etc, all of the nodes within that system are not usually connected to each other. This becomes problematic if you want AI to deliver value since partial data results in lower quality output by AI or even worse, it can come to the wrong conclusions and carry out the wrong actions. So, the IT team will probably need expertise that it hasn’t previously needed in terms of interoperability, model governance, and system integration. This has proven challenging as finding talent that can occupy these roles within a healthcare environment, where information systems and data schema are quite domain-specific is not easy. Most health systems rely on consultants, which introduces more cost. As you can see paying for the AI product is only part of the expenses involved and given the thin operating margins of these institutions, cost is ultimately one of the main barriers to acquiring and launching AI solutions.
Going past the IT department, many innovative healthcare technologies have failed at the point of adoption. This means that the executives bought it, the IT team got it up and running, and it was made available to staff and it never gained much traction. What can explain that? Part of it is that the workflows in healthcare, whether clinical, administrative, or operational, are disorganized and very reactive to the daily events. As such, automation using software has never been easy. Most healthcare software historically have been limited in their capabilities and have not had the ability to handle such an unpredictable environment. Also, much of what happens in healthcare is not in the digital world and integrating into those workflows is challenging. While AI has the promise to overcome these issues since it can handle multimodal inputs, has the ability to reason, and take action, it still will need to be integrated into the existing workflows. If AI is creating a new workflow, it will need to result in significant automation for the staff to adopt those new workflows. All of this will require significant training for the staff that is simulative and interactive so they can feel comfortable with their new workflows. Who will pay for this training? If history is a guide, healthcare organizations will not want to spend this money. That means that the vendors providing these solutions will need to train the staff on the new workflows. This has not been a core expertise of technology vendors. They often do training on the use of their solutions but the end to end workflow training, which is what will drive adoption, has not been done well so far.
So, you need to help the executives find their way in this jungle to choose the right use cases and technologies, then you need to help the IT team with all of the technical issues that need to be handled to implement a solution, and finally you need to train the staff on the new workflows. And, one final step is the ongoing monitoring of the performance of the AI solutions. This will require strong governance committees made up of people from every one of these levels of the organization and tools that will be put in place to help with that monitoring.